
The Seat of the Soul; The Origins of the Autism Epidemic
by ANDREW WAKEFIELD, MB, BS, FRCS, FRCPath
Thoughtful House Presented at Carnegie Mellon University, November 17, 2005
Download this presentation in PDF format.
Where is the seat of the soul? Many men have spent many hours pondering the elusive seat of the soul, including Rene Descartes, who felt that it was in the pineal gland (in the center of the brain--it is responsible for much of our circadian rhythms, amongst other things). He may have been right, he may have been wrong. The seat of the soul may be as elusive as the origins of autism itself. As a gastroenterologist, I am inclined to believe that it's in the intestine, and I'll try to explain why.
A Brief History of
Autism
Leo Kanner first described autism in eleven children in 19431.
The presenting features in patients were so new and so consistent and also so
different from everything that had been seen before that they merited
publication as a new disease syndrome. There were no controls because it wasn't
known what to control against. This is in the nature of the original description
of human disease syndromes. The symptoms as described by Kanner still serve as
the template for our understanding of autism. In spite of the fact that more
than half of the children had clear symptoms of possible intestinal disease, he
interpreted the symptoms as psychologically-based—a misconception that persists
today.
In the 1950s Bruno Bettelheim was considered a leading expert on autism, despite the fact that he had no formal training of any kind (he held a PhD in philosophy). He propagated Kanner's theory that autism was a psychological disorder caused by emotionally cold parents (the "refrigerator mother" theory). As recently as 1981 he wrote, "All my life I've been working with children whose lives were destroyed because their mothers hated them."2 It is tragic that for decades this notion was universally accepted, and indeed it still lingers. A paper written in 2002 (I regret to say from my own medical school) states, "Many children with autism have unusual diets, often associated with constipation, which might lead to non-specific abnormalities of the bowel."3 The implication remains that it's the parent's fault, for feeding the children what they feed them. Kanner and Bettelheim's legacy of blaming the parent hasn't left us altogether.
In the presence of a disease as elusive and enigmatic as autism, it has often surprised me that so many people claim to be experts. We are inundated with "expert" opinion, even though so little is really known about the disease itself. The opinions are many:
Understanding Autism
Where can we begin to untangle this complex disease? The answer is very,
very simple. We must listen to the parents' story. I cannot emphasize the
importance of the clinical history enough. The first lesson I learned on the
ward is that the most important thing to hear is the first thing the patient (or
the patient's parents) tells you. What they tell you gives you the first clue to
their diagnosis. The day you forget that, the day that in your arrogance you
assume you know more than the patient does, is the day you should walk off the
ward and pursue some other career. The patient's history is the starting point.
Only after taking the history and examining the patient can you proceed with
special investigations indicated by the findings. These are the sources that
ultimately lead you to the diagnosis.
There are four features of the clinical history that we have heard from parents again and again, starting in the clinic back in 1995. The first is that the child was developing normally, consistently meeting their first-year milestones. Experts in autism have repeatedly told parents, "Your child was never really quite right. You may have thought they were speaking but they weren't. That wasn't the word ‘helicopter' you heard, it was just a grunt." This is an appalling perception of the accuracy of the parents' view of their own child. Parents know their children--they have known them for thousands and thousands of years. To make the assumption that they did not recognize that their child was not normal is difficult to comprehend. (Alternatively, they tell parents of children who have recovered from autism, "Your child was never really autistic.") In fact, there's a paper that's just come out from the University of Washington indicating that parents are extremely astute observers of their children's development.4
The second feature is regression into autism, often in close temporal relation to a vaccine (usually MMR) or an infectious episode. There has often been a marked clinical reaction to the vaccine, including prolonged high fever and debilitation, from which the child does not appear to recover.
The third feature we hear about is the appearance of gastrointestinal symptoms. When parents first came to me asking for help, I couldn't imagine why they had sought out a gastroenterologist. I knew nothing about autism. But the fact is that at the same time as their regression into autism, these children developed hard neurological and GI symptoms. I will go into the GI symptoms in some detail later. The neurological symptoms were striking--the child would start bumping into things, their gait would become unsteady and broad-based, they no longer wanted to walk upstairs. So it wasn't just that there was developmental regression--disintegration of cognitive faculties--there was also ataxia, a hard neurological feature.
The fourth feature has been reiterated by parents to whom I've spoken around the world—a propensity in autistic children to recurrent upper respiratory tract and ear infections. The rest of the family develops an infection and recovers easily, but the child with autism gets it and can't shake it. The result is a history of multiple antibiotic use going back to the first year of life. I think this may be important in the disease process, or it may be a proxy for an immune system that is not working well.
So if in doubt, examine the patient. We have to look carefully at what's right in front of our eyes. This slide shows us a patient of Dr. Krigsman's. This is what is called abnormal posturing. It's a subtle physical sign that was ascribed previously to maladaptive behavior—to autistic behavior. In fact it is an entirely appropriate behavior. This child has discovered that when he applies pressure to his lower abdomen, it helps to relieve his pain. We now know this because children stop posturing when they receive appropriate bowel treatment.

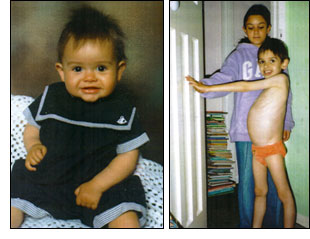 Here's a
little boy I've been seeing in England. Here he is on the left at the age of
one, perfectly happy and healthy, and on the right at the age of six. He looks
like a child from a famine zone in East Africa. He has no muscle mass at all, he
has a hugely distended abdomen--this child has an underlying gastrointestinal
disease until proven otherwise. And yet pediatric gastroenterologists to whom
this child was referred would not see him on the basis that his condition was
too controversial. There is nothing controversial about this child. The person
who is under investigation in this family is not the child, but the mother, for
starving her child. He has two brothers and a sister (behind him in this
picture), and they belie that contention because they are perfectly
well-nourished. This is the awkward position in which medicine has placed
itself—practitioners fail to treat children because of the prevailing dogma,
choosing to blame the parents for the disease instead.
Here's a
little boy I've been seeing in England. Here he is on the left at the age of
one, perfectly happy and healthy, and on the right at the age of six. He looks
like a child from a famine zone in East Africa. He has no muscle mass at all, he
has a hugely distended abdomen--this child has an underlying gastrointestinal
disease until proven otherwise. And yet pediatric gastroenterologists to whom
this child was referred would not see him on the basis that his condition was
too controversial. There is nothing controversial about this child. The person
who is under investigation in this family is not the child, but the mother, for
starving her child. He has two brothers and a sister (behind him in this
picture), and they belie that contention because they are perfectly
well-nourished. This is the awkward position in which medicine has placed
itself—practitioners fail to treat children because of the prevailing dogma,
choosing to blame the parents for the disease instead.
Here is a little girl on the left with whom Dr. Krigsman and I have been concerned. She is perhaps one of the sickest children I have ever met. She manifests several classic features of typical inflammatory bowel diseases such as Crohn's disease and ulcerative colitis. She also has uveitis (inflammation of her eyes), severe arthritis, inflammatory bowel disease, a possible blood-clotting problem associated with a platelet abnormality, severe bruising due to a combination of the latter with self-injury, and regressive autism. Once again it has been exquisitely difficult to get clinical care for this child's physical symptoms, simply because she has autism.
The Gastrointestinal
System
Returning to the question, where is the seat of the soul? My suspicion is
that, if one exists, it is somewhere in the gastrointestinal tract: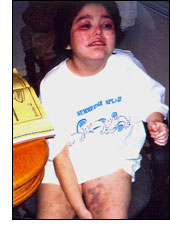
The gastrointestinal tract starts with the esophagus, which leads into the stomach, through the duodenum, into the small intestine, then into the colon (the large bowel), and down into the rectum and the anus. I believe it to be of primary importance in the origins of many cases of autism. Now let's have a look at the lining of the intestine:
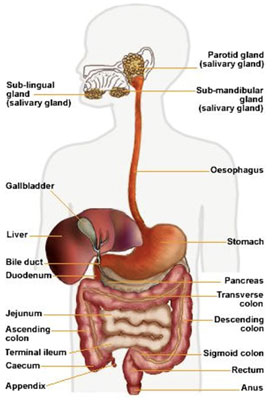
We're looking at the main functional compartment of the small intestine in this slide. Most people are not aware that the intestine is the largest part of the body's immune system. The red peaks in the background as well as the paler peaks you see in the foreground are the finger-like villi; they carpet the lining of the intestine and form the enormous absorptive surface of the small intestine.
The gastrointestinal tract is man's most important interface with his environment. It's full of bacteria, food, and toxins, particularly in the colon. They're usually friendly bacteria that are necessary for good health and immune system function. More and more papers are emerging (specifically from Gibson and Sandler) stressing the important role of intestinal bacteria in normal immune development and function, and the role of these issues in the genesis of developmental disorders.
Autistic Enterocolitis
We published a paper in the Lancet in 1998, describing twelve children
who presented with both GI symptoms and developmental disorders.5 A
follow-up paper confirming this syndrome in sixty children was published in the
American Journal of Gastroenterology.6 Karoly Horvath at the
University of Maryland published a paper describing inflammation in the upper GI
tract of these children.7 Next, there was a series of papers from our
group at the Royal Free Hospital in London characterizing the immunological and
histological aberrations in the intestine of these children, starting in the
colon and then working progressively through the intestine.8, 9, 10
In characterizing the nature of the inflammatory infiltrate in the intestine, we began asking the question, is this similar to diseases that we have seen before or is it different? If it is similar to something we have seen before, where have we seen it?
Dr. Krigsman and his colleagues from New York University School of Medicine presented their research at the International Meeting for Autism Research (IMFAR) in 2004.11 They described the first 147 cases that they had seen, confirming precisely the same disease that we had first described in the United Kingdom. And then more information came from Dr. Federico Balzola in Italy, who presented at the American Gastroenterological Association in Chicago in 200512 and published a paper in the American Journal of Gastroenterology13 describing exactly the same bowel disease in patients with autism from northern Italy. He performed capsule enteroscopy in these children. For the first time, we could see disease of the small intestine that we hadn't been able to see before with traditional endoscopy:
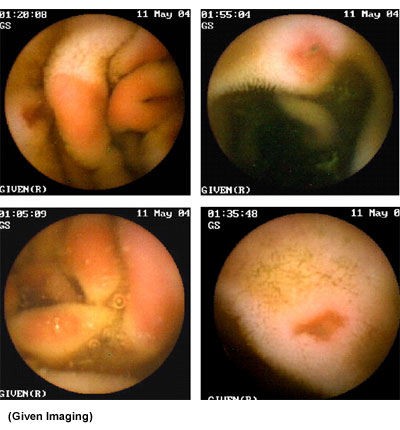
The patient swallows a capsule (or has it inserted using the endoscope) that contains a tiny camera; it passes through the intestine taking two pictures a second.
A further fascinating study suggesting that lymphoid nodular hyperplasia is pervasive across the range of developmental disorders came from Aderbal Sabra, the professor of pediatric gastroenterology in Sao Paolo, Brazil, and Joe Bellanti, professor of pediatric immunology at Georgetown University.14 It showed that the same bowel disease was present in some children with ADHD and ADD, and interestingly in some girls with anorexia nervosa as well. So it may be that for many children across the entire spectrum of developmental disorders there is at the core an underlying gastrointestinal problem.
Replication of these striking findings is ongoing and far-reaching. Just last weekend I was given a paper that was presented to the Venezuelan Society of Perinatology and Pediatrics by a pediatric immunologist who won first prize for his efforts. He found inflammatory bowel disease in 100% of the autistic children studied.15 So this idiosyncratic bowel disease is seen all around the world in children with a variety of developmental disorders. It has been gratifying to watch the replication unfold since our first observation.
What have these studies shown? Firstly that there is expansion of the lymphoid follicles, particularly in the small intestine, in addition to lymphoid nodular hyperplasia. Rather like having a lymph gland in the neck that swells up when you have a sore throat, the lymph glands in the intestine swell enough that they encroach upon the lumen of the intestine, and in this way may be responsible for partial obstruction and pain (rather like having a throat so sore that it hurts to swallow anything). This is also associated with an increase in the number of inflammatory cells and immune cells within the intestine. There appears to be an autoimmune attack against the lining of the intestine. In association with this we get a compromise of the barrier function of the intestine. There are digestive enzymes on the surface of the villi, which are essential for the normal digestion of food and the maintenance of intestinal health. When these enzymes are not working properly--as in children with various infectious enteropathies (following a rotavirus infection, for example)--then the consequence may well be malabsorption and diarrhea. The presence of undigested food in the stool is something that we commonly see in these children. This has been demonstrated in children with autism both by Dr. Tim Buie at Harvard16 and by Karoly Horvath.17 We also see ulceration—the breakdown of the lining of the intestine. There is dysbiosis, which is an overgrowth of potentially pathogenic aerobic and anaerobic bacteria in the colon and in the small bowel. This reportedly leads to the proliferation of Paneth cells as a source of antibacterial peptides. This is the constellation of pathology in the intestine that forms the disease we now call autistic enterocolitis.
We also see grossly disordered cytokines in these children.18 These are the chemicals that mediate cross-talk among immune and other cells, or regulate the inflammatory process. For example, in this slide, we can see tumor necrosis factor-alpha-producing cells (TNFα) at an unexpectedly high level in the intestinal lining, compared with developmentally normal controls:
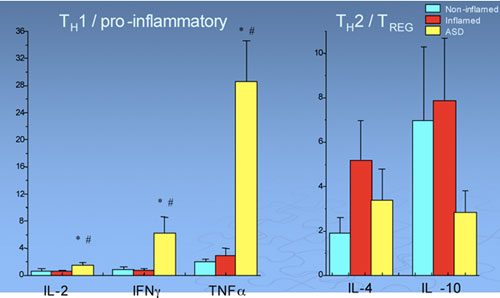
TNFα is a very powerful pro-inflammatory mediator, and we'd usually only expect to see levels this high in children with Crohn's disease. There is also an increase in interferon gamma (IFN-γ), which is a major pro-inflammatory mediator. On the other side of the equation, in children with autism we see a diminution of interleukin-10 (IL-10). IL-10 is the anti-inflammatory--it's like the aspirin of the immune system. So as you can see, there is a gross imbalance between the pro-inflammatory drive and the anti-inflammatory molecules in children with autism that you don't see in other inflammatory bowel diseases or in normal children. The ratio of pro-inflammatory to anti-inflammatory molecules, for example IL-12 to IL-10, clearly distinguishes these children and may be a biological marker of this derangement. We do not see this same pattern in other inflammatory bowel diseases.
A paper from Becker at the National Institutes of Health casts light on the genetic contribution of the dysregulated immune function.19 Becker examined the idea that if autism is an autoimmune disease, then there should be overlaps between the genes that encode for susceptibility to autoimmune diseases such as colitis, rheumatoid arthritis, or lupus, for example, and autism. And he looked at genome-wide scans and made these comparisons. His review of the literature in this respect was fascinating: "...of particular note, given suggestions of bowel inflammation in autism, are co-localization of markers including identical markers linked to both autism and celiac disease (a primary inflammatory bowel disease associated with an allergic sensitivity to gluten), and autism and Crohn's disease." The results suggest that in this group of autistic children we are looking at a new variant of inflammatory bowel disease that shares common genetic susceptibility determinants with other known inflammatory bowel diseases.
A Primary
Intestinal Disease?
The data suggest a primary inflammatory bowel disease in many of these
children (clearly not all children with autism, but certainly a large percentage
of the children with the regressive type of autism). Have we seen this bowel
disease—a combination of LNH and mucosal inflammation--before? We have seen
something very like it, and that is in HIV enteropathy. When we examine the
intestine in patients who are known to be infected with HIV, we find no other
cause for their enteropathy (such as cryptosporidium, for example), and yet what
we do find is HIV and a very similar pattern of inflammation. What this suggests
to us is that the bowel disease we see in children with autism is consistent
with a viral cause.
What is driving the intestinal pathology? For the first time we have a starting point, and that is the swelling of the lymph glands within the intestine. We know that if we take a patient with HIV infection and we biopsy those lymph glands and stain a section of that biopsy with an antibody against one of the HIV proteins, we find the HIV antigen. If we take a patient with new-variant Jakob-Creutzfeldt disease (mad cow disease) and we look for prion protein in the intestine of these patients, we find the prion agent in the center of those reactive lymphoid follicles. So we are developing our ideas based upon known human disease syndromes.
If we take a patient with acute measles virus infection who has diarrhea and we scope and biopsy them, we find the measles virus protein in the intestine, causing lymphoid hyperplasia. When we take a biopsy from the gut of a child with autism and we stain it with an antibody that is specific for measles virus, we find it in the same place. If we take World Health Organization reference monoclonal antibodies against measles virus that have been extensively tested for specificity and apply them to the same tissues, we find the same thing. If we take those antibodies and look at those tissues disaggregated into single cells by a technique called flow cytometry, we find the same thing. And so the measles virus protein appears to be present in these reactive lymphoid follicles. I stress that that does not make it the cause of autism, but it makes it an interesting candidate. When we look for other viruses such as adenovirus, herpes simplex 1 and 2, HIV, mumps, rubella--we don't find them in these kids--we find measles.
Professor John O'Leary in Dublin did a large study (ninety-one children) using the latest molecular technology in order to find out whether not just the protein but also the gene of the virus is present in the intestine.20 Measles virus genomic RNA was present in seventy-five of those children (82%), compared with 7% of seventy developmentally normal controls. At the very least, this confirms a statistical association between the presence of the virus and this disorder. Again, this is not a causal association, it is a statistical association.
If it were causally associated with measles virus, then what would we expect? We would expect there to be a historical association between measles exposure and developmental disorders. In 1956, at the Section of General Practice in the Royal Society of Medicine, Dr. Daynes stated: "Typically a child between one and five years becomes naughty and difficult a few days after the onset of an acute infectious illness…. such as measles or gastroenteritis…. he's irritable, negativistic and spiteful, sleep is disturbed and he wakes up in the night and often screams: his appetite is poor, he fails to gain weight, his abdomen is often distended and the stools may become bulky, pale, and offensive." Does that sound familiar? Dr. Daynes continued, "The study of over forty cases has led me to formulate a syndrome, pre-celiac syndrome… This condition, if left untreated, usually rights itself after a month or two, but it may last for much longer in which case slight petit mal attacks may develop in addition to worsening of the other symptoms…. I have been placing these children on a gluten-free diet at the earliest opportunity and the symptoms respond dramatically, usually within two or three days. They relapse if a premature return to a normal diet is made."21
Further on the historical association, in 1979 at the Harvard School of Public Health, Deykin and MacMahon showed that atypical patterns of exposure to measles, mumps, and rubella (perinatally or in utero) are associated with autism in the offspring.21 Ring and Barak from Israel have shown that children born during epidemics of measles are at greater risk of autism. And so these historical associations provide the rationale for pursuing this line of research.
Measles Virus: Effects on the Immune System
If developmental regression were associated with measles, what would we
expect in terms of the immune system response? We need to look at what we know
about the immune system and the effects of measles upon it. Because measles is
profoundly immunodisruptive or immunosuppressive, following the induction of
measles antibody we would expect that the lymphocyte numbers and function in the
blood might be depressed. We would expect that there would be a decrease in the
response of lymphocytes to provocation from antigens such as tetanus, for
example, and that, paradoxically, the immune system would be in a state of
chronic activation. Certainly we find lymphopenia:
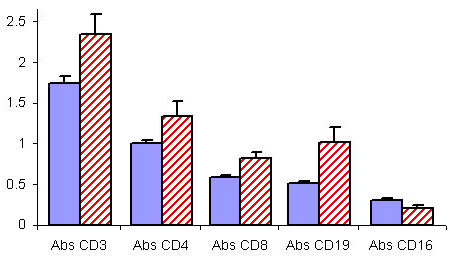
This graph shows the levels of various immune cell populations in the blood of children with autism (blue), and developmentally normal children (red). Levels of all of these immune cells, with the exception of CD-16 natural killer (NK) cells, are significantly lower in the autistic children. Elevation of the number of NK cells in these children is a common finding. When we look at the function of NK cells (anti-viral cells), however, we see that although they may be increased in number, they are depressed in their activity, i.e., their ability to kill target cells.
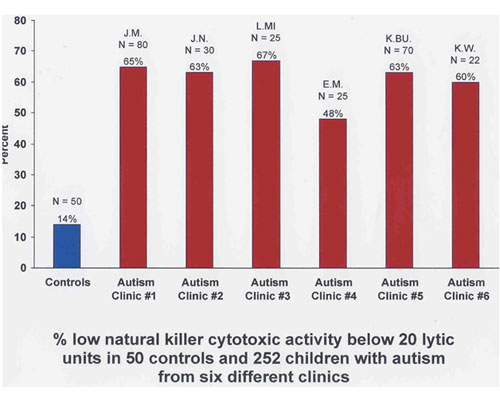
These data from six autism clinics across the US (provided by Dr. Elizabeth Mumper) look at the percentage of children with low natural killer cell cytotoxicity (killer activity) compared with developmentally normal controls:
Another fascinating study, which really re-defined the way we look at anti-viral immunity and its induction, comes from Dr. Appay and colleagues at the University of Oxford. These authors looked at the differentiation of antiviral (CD8) cells following exposure to, and subsequently during the chronic phase of, certain viral infections, including HIV, Epstein Barr virus, and hepatitis C virus. Specifically, they examined the expression of molecules CD38, CD27, and CD28 on the surface of CD8 (anti-viral) lymphocytes as a marker of their differentiation status.23
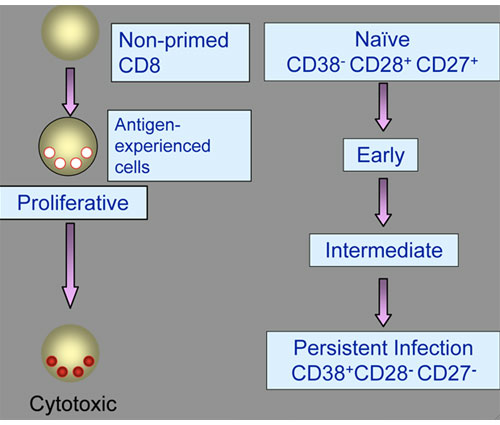
We start with a naïve CD8 T cell that has never seen a virus. It's like a new recruit in the army. We then expose it to a virus and it differentiates to become the fully cytotoxic activated CD8 T cell. As that happens, the cell changes expression of the molecules on its surface to become CD38-, CD28+, and CD27+. In the persistent phase of the infection, when the body has failed to clear the virus, there is an excess of these cells seen in the blood. The continued expression of these molecules seems to represent a state of chronic viral activation and exhaustion of the ineffective antiviral T-cells. Therefore if we are looking in these children for evidence of a persistent viral infection, we should expect to see an excess of this population of cells. When we look at these cells in children with autism compared with both non-inflamed and inflamed developmentally normal controls, that is precisely what we find. The data are certainly consistent with chronic immune system activation associated with a persistent viral infection. In other words, the immune system under normal circumstances is vigorous and causes viruses to wish they had not invaded the body. However, under certain circumstances it may fail in its mission to get rid of the infection. This frustrated response can be associated with an autoimmune attack directed against the host, as is often seen in AIDS.
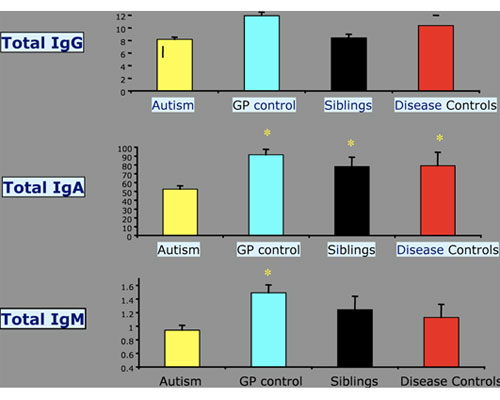
Next question: is there a specific antiviral immune response in children with autism? Dr. Singh at the University of Utah Medical School has now published three papers showing consistently abnormal antibody profiles with an elevated measles virus antibody titer in children with autism, compared with controls, that is not seen for antibodies against other common viral infections.24, 25, 26 ames Oleske at the University of Medicine & Dentistry of New Jersey (UMDNJ) has found the same thing, as has Paul Ashwood at the University of California/Davis. Dr. Ashwood took a large group of children with autism and a similar number of controls, and looked at their total IgG, IgA, and IgM antibody titers in the blood. He compared these with general population controls, sibling controls, and disease controls. First he showed that there were low levels of circulating antibody in the blood of children with autism compared with controls, as has been reported by others:
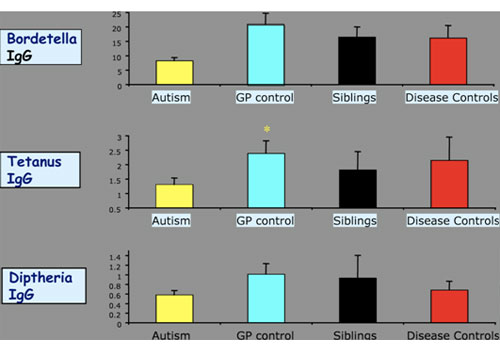
Then, when he looked at antibodies to common antigens, in this case the vaccine antigens of pertussis, tetanus, and diphtheria, he found they were depressed in the children with autism, consistent with the low levels of IgG:
Again, with common environmental agents such as CMV and influenza A and B,
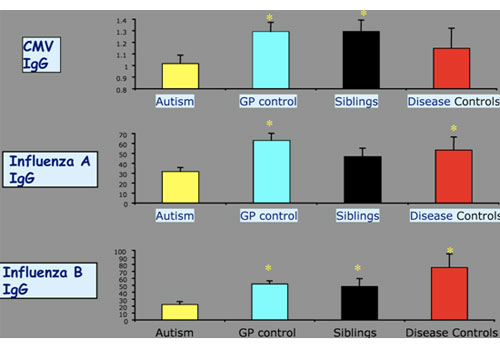
they were depressed in the children with autism. And yet when he came to the antigens of measles, mumps, and rubella, they were elevated in the children with autism:
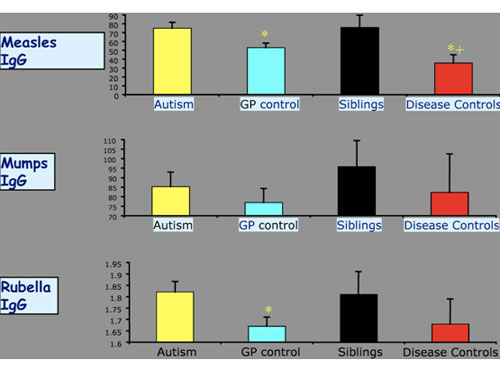
Low antibody titers were also seen against common environmental infections such as CMV (Cytomegalovirus) and influenza A and B. These were also depressed in the children with autism. And yet when he looked at antibodies against measles and rubella, these were elevated in the children with autism.
In summary, at this stage what we have is a novel intestinal disease in these children consistent with a viral etiology, and at least the suggestion of a measles virus source that needs to be resolved in follow-up studies.
MMR
How do we determine whether the association between MMR vaccine and
autism is causal or not? One way is to compare the effects of different brands
of the MMR vaccine to see if there is a systematic difference in the pattern of
autism among brands. In the UK, unlike the US, three brands of the MMR vaccine
were introduced simultaneously in 1988: MMR2, Pluserix, and Imravax. The adverse
reaction profiles of the three vaccines were different--indeed, two of them were
withdrawn because they caused meningitis due to the particular strain of the
mumps virus. So given that the different brands of MMR had different adverse
reaction profiles, we were able to form the hypothesis that if there is no
relation between MMR and autism, there should be no systematic differences
between MMR vaccine brand and autism phenotype, recovery, and associated
features such as immune status, bowel disease, and persistence of the measles
virus.
In fact Pluserix, the vaccine that was withdrawn, was associated with a significantly greater risk of measles virus persistence as detected by TaqMan PCR in both the bowel tissue and in the blood, compared with MMR 2. Pluserix and measles virus persistence were associated with lesser degrees of recovery from autism. The presence of measles virus in the intestine predicted the presence of measles virus in the blood, and the presence of measles virus was also associated with more obvious immunodeficiency. These data suggest that an effect of brand predicts an effect of the vaccine.
By way of contrast, I want to draw your attention to a study conducted by Dr. Smeeth and colleagues in the UK. They predicted that if MMR were linked to autism, there should be a higher rate of MMR uptake in autism cases compared to non-autistic controls. In a letter to The Lancet in 1992, they stressed the importance of looking at the regressive subgroup. Smeeth et al. understood that the key question is whether MMR vaccine exposure is linked to autism of the regressive subtype. However, when it came to publication of their paper two years later, the subgroup of patients with regression was not identifiable, because they lumped them all together. The paper fell at the very first hurdle.27
But there was an even more significant problem--the matched design analysis they chose to use required that if they were going to be able to detect a difference (if indeed there was a real difference) they would need a wide disparity in MMR vaccine uptake between cases compared with controls. They used a conditional logistical regression analysis, which works by removing cases and controls with the same exposures. First you take out the matched cases and controls that both got MMR, and then you take out the matched cases and controls that did not get MMR, and then you analyze what is left. So rather than having a study of 1,500 children with autism, as we were led to believe, the analysis was actually conducted on a very small proportion of those cases because of the striking similarity in vaccine uptake between cases and controls—the study did not have sufficient power to detect a difference even if one existed. The authors must have known this from the outset. If an association between MMR and autism genuinely existed, then in order to detect this association, the study would have needed between 8,000 and 40,000 cases of autism, rather than 1,500. The study should never have been published. And yet it is precisely this paper that the British government refers to and relies on when they say the investigation of the relationship between autism and MMR should be concluded.
In summary, many children with developmental disorders have a systemic disease with an underlying and potentially primary inflammatory bowel disease. The disease has the features and characteristics of an infectious cause. In some children with autism, there may be a link between primary GI inflammation and secondary central nervous system immune activation and tissue injury. Plainly there is convergence of biological evidence towards causation. It is far from being there yet, but this is most certainly not the time to stop looking. My opinion on MMR vaccine safety is shared by Dr. Jefferson whose paper, published in the journal Vaccine, stated, "The design and reporting of safety outcomes in MMR vaccine studies, both pre- and post-marketing, are largely inadequate," and "We found limited safety of MMR compared to its single-component vaccines from low risk of bias studies."28 These are not my words. I am wholly in favor of protecting children against infectious disease with the judicious use of vaccines that are safe and effective. Nonetheless I do believe that with certain vaccines, such as MMR, there were shortcuts taken which were imprudent.
Mercury
What is the role, if any, of mercury in autism? Let me present to you one
biologically plausible example of how thimerosal and other toxic exposures might
influence the risk of autism in the context of an infectious cause. In the
Russian steppes there is a very interesting ground squirrel. This little
creature may tell us a great deal about the origin of autism. He carries in his
throat the organism for plague (yersinia pestis), and he can live year on year
in the steppes carrying this organism in his throat with no problem at all. Just
down the road, however, whole colonies of his colleagues die in annual epidemics
of plague. Why is this agent benign in some areas and in other areas a pathogen
that kills? The Moscow Institute of Ecology and Evolution put forward the
hypothesis that it was actually the toxic metal content of the forage plants
they were eating that predicted whether this agent was going to be a harmless
freeloader or a killer. They tested this hypothesis in a sixteen-year study and
demonstrated precisely that. Where animals were dying, there was an excess of
toxic metals and/or a deficiency in metals beneficial to the immune system,
compared with other areas where the organism was benign. They suggested that the
toxic metals interacted with the immune system and turned the plague organism
into a pathogen. This was a fascinating ecological study on the synergistic
interaction of potential etiological or causative agents.29
In the laboratory, we see the same thing. Let's look at mercuric chloride. Here we see an animal that, by virtue of his genetic makeup, is protected against the pathological effects of leishmaniasis. But another, who is genetically susceptible, develops immune disease when you give him leishmaniasis; he can't clear the pathogen, and he may die. However if you take this genetically resistant animal and give him sub-toxic doses of mercuric chloride and then give him leishmaniasis, he too succumbs to immune disease.30 Interaction between two agents in the environment potentiates the effects of the infectious agent.
Thimerosal, the ethylmercury-containing preservative recently used in childhood vaccines, produces the same phenomenon in mice.31 Thimerosal has initial immunosuppressive effects similar to those of methyl mercury. However, in contrast to methyl mercury, thimerosal treatment leads to a second phase with a strong immunostimulation and T-cell dependent IFN-? and IL-4 mediated autoimmunity in genetically susceptible mice. And so there it is, it can happen. There is biological coherence.
I believe that in these children, for genetic or environmental reasons, the immune system is compromised, which may then lead to an increased risk of an adverse response to a vaccine. Despite the emerging coherence, the Institute of Medicine (IOM) said, " STOP—no more research regarding thimerosal or vaccines is necessary." I fail to understand how in heaven's name, faced with those data, they could possibly have come to that conclusion. This is an extraordinary situation.
The IOM based their position not upon the biological data or the clinical findings that were emerging in affected children, but on the population-based studies that had failed to find an association. Let's look at some of those studies (I owe a debt of gratitude to Mark Blaxill for providing this analysis). Let us look first at the prevalence of autism--the number of children affected in the population. Data presented by Dr. Eric Fombonne suggests that the situation is very confusing and therefore it is uncertain whether the prevalence is rising or not. Dr. Fombonne presents the data by year of publication. It is uncertain why one would ever present data by year of publication since it tells you nothing whatsoever about the population represented in those papers, and inevitably causes confusion.
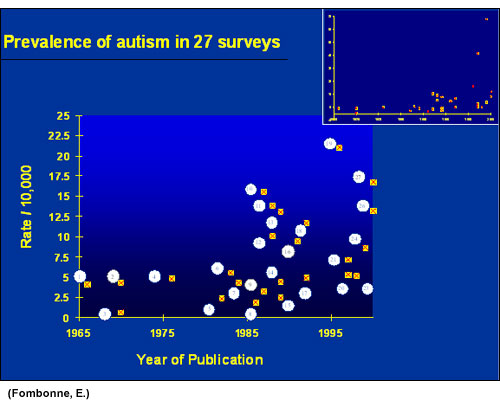
However, when you take the data from these studies and hold age (mid-point year of birth of subjects in the study) constant, a much clearer picture emerges. That is, a striking upward trend in the prevalence of autism in children born in the US in the mid to late 1980s and in the UK in the same time period:
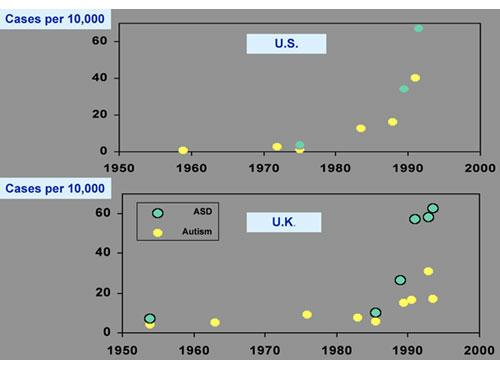
If alternatively one holds geography constant (looking at, for example, California) and graphs autism by age group, a similarly clear pattern emerges. Autism is uncommon in twenty-one year olds, but it is becoming increasingly common in the younger age groups. (Of course, the numbers fall off in the youngest children, many of whom have not yet been diagnosed.) In this way one can dissect out the true trend in disease prevalence.
Let's consider hypotheses that have been put forward to account for the increasing prevalence of autism, and how they have been dealt with. One of the earliest was the hypothesis of diagnostic oversight ("We just missed the cases in the past"). Several studies have now examined this issue, and determined that diagnostic oversight cannot account for the rise.32, 33, 34, 35
Then there is the hypothesis of diagnostic substitution. It has been suggested that children are being diagnosed with autism when previously they would have been diagnosed with mental retardation. This should lead to a rise in the diagnosis of autism and a diminution of the number of children being diagnosed with mental retardation. Croen et al. published findings that claimed to demonstrate diagnostic substitution36, but subsequently had to print a retraction of their interpretation37 after it was clearly demonstrated38 that diagnostic substitution did not account for the changes.
What about the possibility that the increase was caused by diagnostic broadening--that we have broadened the diagnostic concept of autism and therefore we're including more children? In fact in 1994 there was what was called a "corrective narrowing" of the DSM-IV, the diagnostic criteria, and yet the incidence or the prevalence of autism has continued to increase. Furthermore, the MIND Institute at UC/Davis published a detailed report refuting this theory.39 So these hypotheses have been examined and not one of them has held up to close scrutiny.
Primary
Inflammatory Bowel Disease?
Are we looking at a primary inflammatory bowel disease--a systemic
disease that has secondary consequences for neuroimmune system function? Can a
primary inflammatory bowel disease lead to secondary activation of areas in the
brain that are involved in autism? This hypothesis was tested by Martha Welch
and colleagues at Columbia University, who looked at an animal model of IBD
induced by trinitrobenzene sulfonic acid (TNBS).40 This is a standard
experimental model of inducing intestinal inflammation. In post-mortem brain
sections, Dr. Welch looked for evidence of immediate-early gene activation (Fos),
which was increased in certain areas of the brain that are known to be important
in autism, such as the amygdala. This was not seen in control animals that had
saline exposure instead of TNBS. This same model has been used to demonstrate
other central nervous system changes in response to primary intestinal
inflammation, including increased blood-brain barrier permeability and central
autonomic activation that is independent of the vagus nerve.41 So in
answer to the question: can a primary intestinal inflammation cause secondary
brain activation? The answer is yes.
Next question: what might be the consequences of such secondary activation in the brain? An important paper in this respect comes from Vargas and colleagues at Johns Hopkins.42 The study looked for evidence of immune activation in the brain and spinal fluid of patients with autism and in controls. The principal cells of interest were microglia cells, which form part of the resident innate immune system of the brain. Vargas and colleagues showed activation of these cells in areas of neuronal damage. This slide shows control cerebellar cortex from a non-diseased post-mortem specimen (A), and tissue from the patient with autism (B), that highlights damage to the Purkinje cell layer of the brain in association with adjacent microglial activation. This HLA-DR molecule (C) expressed on the surface of microglia is a marker of activation of the resident innate immune system:
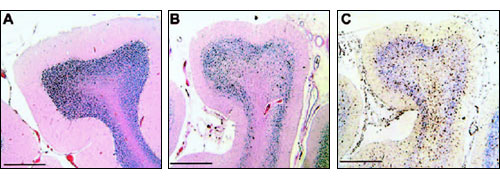
The source of the activation of the microglia was not evident; nor was there evidence of infiltration of the brain by inflammatory or immune cells from the blood. However, what they found in the spinal fluid were high levels of certain inflammatory cytokines, including IFN-?, derived from lymphocytes. Yet there were no lymphocytes in the brain tissue and no excess of the cells in the spinal fluid. The conclusion of Vargas and colleagues, and indeed our own conclusion, is that the cytokines are coming from somewhere else. Vargas did not consider a source outside the central nervous system. (Ironically, in the very same week that they published, we also published a paper in the Journal of Clinical Immunology showing these same cytokines coming from the inflamed intestine.43)
Is it possible that what we are observing is a systemic inflammatory response from the intestine leading to secondary immune activation in the brain, and cell damage? We've seen this before, in celiac disease--a primary immunopathology of the intestinal mucosa associated with an allergic sensitivity to gluten. Celiac disease is associated with a wide variety of secondary neurological complications, including autistic behavior, dementia, peripheral neuritis, focal and generalized seizures, and cerebral calcification.44 Celiac disease provides a perfect example of a primary gut disease leading to secondary brain damage. Placing patients on a gluten-free diet may lead to some amelioration of these neurological features.
Convergence and
Consolidation
Finally, what we have at this stage in autism research is peer-reviewed,
published literature demonstrating a convergence of biological findings
concerning a possible mechanism and cause in some children. We've known for some
time, both anecdotally and from one single-blind, randomized, controlled study
that a gluten-free diet can produce amelioration of behavioral symptoms in
children with developmental disorders. While this may be related to an opioid
phenomenon, we are also aware, from the work of Dr. Jyonouchi at UNJMD, that
peripheral blood immune cells of these children are hyper-responsive to peptides
derived from gluten and milk proteins, in terms of pro-inflammatory cytokine
production. This finding was particularly the case in autistic children with
gastrointestinal symptoms, and it provides a further biological rationale for
the efficacy of a gluten-free, casein-free diet in such children.
Data from the laboratory of Jill James and colleagues from the University of Arkansas indicate that there is oxidative stress in these children, associated with depletion of reduced glutathione.49 Then we have the observation that a primary inflammation of the intestine, as seen in celiac and TNBS-induced colitis, can produce secondary brain changes, and finally there is the Vargas study showing neuroglial activation in the brain.
And so you can see that although science, like nature, appears to abhor consensus (preferring diversity, at lead initially), there is a growing consensus and consolidation of information, a coherence about what appears to be happening in these children with autism: intestinal immunopathology, a proinflammatory cytokine profile, a hyperimmune response to dietary proteins, dysbiosis, autoimmune phenomena, and possible opioid toxicity.
From the historical perspective we have a body of evidence supporting an association between measles virus and developmental disorders, including autism. We also have the demonstration of an abnormal immune response to the measles virus, and more recently, in Medical Veritas,50 the demonstration that in children who have had two shots of the MMR vaccine instead of just one, the bowel disease is worse—in other words, we see a biological gradient effect in these children.
But as we know, causation is rarely simple. More work is needed.
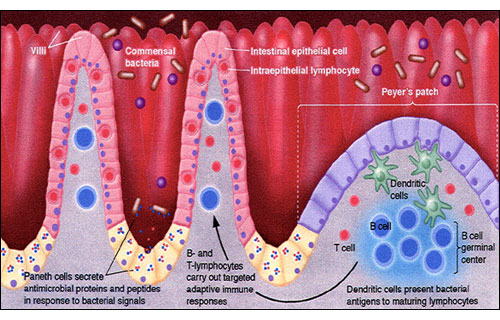
So, where is the seat of the soul--in the bowel or the brain? It's the wrong question and always was. This little boy holds the answer. He looks extremely well now (left), and he is certainly getting better, but if you look at an old picture of him (right) you see something entirely different:

This is a picture of a self-injurious child who has damaged himself in an attempt to escape extraordinary abdominal pain--pain that he had lost the ability to communicate. His mother instinctively knew he was suffering, yet could not convince anyone in the medical profession to respond appropriately. Because his mother treated his underlying gastrointestinal disease appropriately and diligently (by a special exclusion diet) we now have the Superman that you see on the left. This child is the seat of soul – the soul of this Nation.
So I appeal to the conscience of this great country: unless we take this sufficiently seriously, unless we address this issue now, unless we prevent the subversion of the scientific process in favor of political and financial expedients, then we are in terrible trouble. Vaccination policy is nothing more than words on paper without public confidence. If we undermine confidence in the vaccination program by sticking our heads in the sand, then we have done children everywhere a huge disservice.
Autism is a national economic and spiritual emergency, one that will tear the very fabric of society if we let it. It is a world emergency, and we need to start treating it as such. I leave you with the words of Ronald Reagan, who said "…government is never more dangerous than when our desire to have it help us blinds us to its power to harm us." In this instance, I, for one, take that to heart.