Cytotec/Misoprostol Obstetrics and Gynaecology
Birth
trauma
INDUCTION WITH CYTOTEC/MISOPROSTOL IS KILLING WOMEN AND
BABIES
Jeanice Barcelo
SUNDAY, MARCH 3, 2013
http://birthofanewearth.blogspot.co.uk
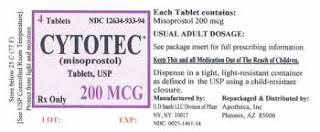
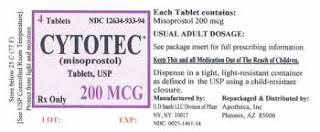
Cytotec/Misoprostol is a ulcer drug. Despite the fact that the makers of this
drug have warnings on the label saying the drug should not be used during
pregnancy, it is nevertheless being used off-label in hospitals every day to
induce labor and force babies to come before they are ready. It is an extremely
dangerous drug and is killing women and babies.
"...misoprostol is associated with an increase in meconium staining, uterine
hyperstimulation, uterine rupture, amniotic fluid embolism, maternal mortality,
perinatal mortality and hypoxic ischemic encephalopathy of surviving infants....
Although hard data cannot be found on the number of uterine ruptures following
misoprostol induction in the United States, an Internet organisation has
identified over 380 women who have had uterine rupture, many following
misoprostol30 and there is considerable anecdotal evidence that many babies
died...
a number of law suits have alleged that negligent induction of labour with
misoprostol has damaged the baby and/or the mother. There are no known
systematic data on cases of litigation associated with misoprostol induction but
at least 16 cases have been reported,22 and all suits known to have been
resolved to date have been settled in favour of the plaintiff...
Full article here:
"Drugs are licensed to treat specific conditions but
doctors can use them for other reasons so long as they take responsibility. This
is called ‘off-label’ use. Sometimes the drug has not been submitted to the
regulatory system for the indication, other assessment has revealed that use for
this indication is contraindicated. Such ‘contraindicated’ use is probably a
greater risk than ‘off-label’.
Doctors use drugs off-label if they are convinced their patient cannot wait for
regulatory approval, there is no other available licensed drug, if they judge
that the benefits outweigh the risks or sometimes just because the unlicensed
drug is cheaper.1 The practice is common in obstetrics. In one survey2 of 731
birthing women, 23% had received off-label drugs. Such prescribing is rarely
controversial. Of the 10 off-label drugs in the survey, only one, the use of
misoprostol for labour induction, the subject of this commentary, carries
serious risks.
Misoprostol (prostaglandin E1) is marketed as Cytotec for the oral treatment of
peptic ulcers. It has uterotonic activity but is not only unlicensed for use in
pregnancy but labelled as contraindicated in pregnant women. Nevertheless, it
has been used for the induction of labour since the 1990s.
This off-label use is unusual, in that other related products such as
dinoprostone (prostaglandin E2) and oxytocin are licensed for labour induction.
It was also potentially hazardous because early prescribers did not know the
correct dose or the suitability of the oral formulation for vaginal use. The
research they conducted to find out was relatively haphazard, and few patients
were informed that they were receiving an unlicensed drug.
Indirect evidence suggests that many American women have been given misoprostol
for labour induction. Induction of labour was used in 18% of births in 19983
approximately 720,000 inductions annually and in at least two large US
hospitals,4 it was the most common agent used. It has been described in the
media as ‘the drug of choice for induction of labour’.5 It has also been widely
used to induce labour in women with a previous caesarean section.6 In Portland,
Oregon it was used in 60% of patients with previous caesarean deliveries who
underwent induction of labour between 1996 and1998.4
Prelicensing studies normally consist of randomised trials performed to the
standards of the International Conference on Harmonisation Good Clinical
Practice (ICHGCP).7 This never happened with misoprostol for labour induction.
Instead, doctors experimented with the dosage, either by informally ‘trying out’
the drug or performing small trials with idiosyncratic research protocols,
eventually accumulating sufficient data to assess efficacy. The tablets came in
unscored 100 μg and scored 200 μg tablets, so clinicians first tried one 100 μg
tablet every 4 to 6 hours, either orally or vaginally. When uterine
hyperstimulation and the occasional uterine rupture occurred, the dose was
reduced by cutting the 100 μg tablets into halves or quarters, and by 2001, the
consensus was for 25 μg (1/4 tablet) given vaginally every 4 to 6 hours.8 Even
now some hospital pharmacies decline to cut unscored tablets due to the inherent
inaccuracy of dose.
Vaginal pessaries are normally formulated differently to oral tablets. They are
shaped for ease of insertion and use different excipients including different
binders, fillers, lubricants, disintegrants. Using an oral tablet vaginally
results in a different pharmacological effect. Vaginal application of
misoprostol results in slower increases and lower peak plasma concentrations
than oral, but overall drug exposure is increased.8 With vaginal insertion, the
plasma concentration remains near peak levels 4 hours after insertion.9
Researchers also compared misoprostol with oxytocin,10 with dinoprostone
(prostaglandin E2) gel11–13 and dinoprostone vaginal inserts,14–16 as well as
oral and vaginal use.17–19 However, no trial was of sufficient size to measure
or compare reported rare but serious risks such as uterine rupture, amniotic
fluid embolism or neonatal and maternal mortality.4,6,10–15,17,18,20
Despite the fact that off-label users may be less inclined to report adverse
effects to the authorities, preliminary data suggest that misoprostol is
associated with an increase in meconium staining, uterine hyperstimulation,
uterine rupture, amniotic fluid embolism, maternal mortality, perinatal
mortality and hypoxic ischemic encephalopathy of surviving
infants.4,6,8,10–16,19–27 There are many other examples of tragedies following
the widespread use of procedures or drugs before adequate scientific evaluation,
such as routine prenatal X-ray pelvimetry, di-ethylstilboesterol and thalidomide
during pregnancy.
Small trials and lack of standardisation of research protocols has made
meta-analysis unreliable.25 The editor of this journal, commenting on a
misoprostol induction trial in January 2004 wrote: ‘Previous trials have been
too small to provide clear evidence on rare but important outcomes such as
uterine rupture, and even in the present larger trial there was only one uterine
rupture in each group’.27 One review admits: ‘the relative risk of rare adverse
outcomes with the use of misoprostol for induction of labour remains unknown’.8
and the latest Cochrane review laments that ‘The studies reviewed were not large
enough to exclude the possibility of rare but serious adverse events,
particularly uterine rupture, which has been reported anecdotally following
misoprostol use in women with and without previous caesarean section’.21
The situation with misoprostol induction after caesarean is complicated by the
fact that other prostaglandins are not licensed either, so the extent to which
complications such as uterine rupture result from misoprostol itself or from the
use of prostaglandin in general remains unclear.8 Two articles suggest a higher
risk of uterine rupture with misoprostol induction than for the other
prostaglandins.4,6
Normally, patients given an experimental drug, whether in a formal trial or in
an uncontrolled way, are fully informed and given written consent. However,
patients prescribed off-label are rarely told, and the American College of
Obstetrics and Gynecology has said that informing patients is up to the
discretion of the clinician.28 Many patients appear to have been just told that
it was ‘safe’. The patient information sheet at one UK hospital stated in 2003
(Sheila Kitzinger, personal communication): ‘Many pregnant women world-wide have
used misoprostol for labour and shown it to be safe for you and the baby’.29
Among 16 patients experiencing adverse outcomes after misoprostol induction in
the United States,22 none had been informed that it was not approved although
they had been told it was ‘safe’. In interviews on national television, women
with uterine rupture after misoprostol induction have claimed to have not been
informed that the drug use was off-label.5
The lack of informed consent matters. Although hard data cannot be found on the
number of uterine ruptures following misoprostol induction in the United States,
an Internet organisation has identified over 380 women who have had uterine
rupture, many following misoprostol30 and there is considerable anecdotal
evidence that many babies died.4,6,8,16,19,21–24 In a case–control study of
uterine rupture in 512 women attempting vaginal birth after caesarean section,4
5.6% of the women in the misoprostol group had symptomatic uterine rupture, as
compared with 0.2% of the women undergoing a trial of labour without the
administration of misoprostol (P < 0.001).8 At least four women have died after
misoprostol induction of labour, all with postmortem findings consistent with
amniotic fluid embolism.20,22–24 To date, published trials are too small to
calculate the rate of uterine rupture and the rate of amniotic fluid embolism in
labours induced with misoprostol on an unscarred uterus, although a warning of
both risks is included in the package insert and in a letter from the
manufacturer Searle to doctors.26 Perhaps unsurprisingly, a number of law suits
have alleged that negligent induction of labour with misoprostol has damaged the
baby and/or the mother. There are no known systematic data on cases of
litigation associated with misoprostol induction but at least 16 cases have been
reported,22 and all suits known to have been resolved to date have been settled
in favour of the plaintiff. In late 1999, the American College of Obstetricians
and Gynecologists came out against misoprostol use with a scarred uterus but not
against its use for induction on an intact uterus. In 2000, Searle, the
manufacturer of Cytotec, at the request of and in close collaboration with the
FDA,26 wrote to all American physicians reminding them that using it for labour
induction was contraindicated, listing the adverse effects reported to them and
the FDA and urging them not to use it for labour induction. Most other expert
committees including those of the British Royal College31 and the Canadian
Society32 have concluded we do not yet know enough about the risks of
misoprostol induction to use it, except in approved experimental trials with
fully informed consent."
Source Article
Off-label use of misoprostol in obstetrics: a cautionary tale
http://onlinelibrary.wiley.com/doi/10.1111/j.1471-0528.2004.00445.x/full