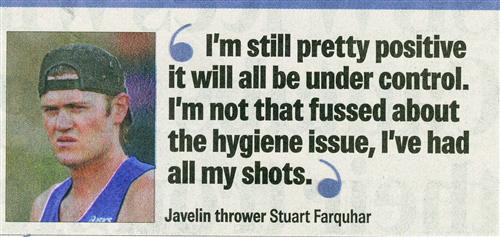
 I've
had all my shots." So said Javelin Thrower Stewart Farquhar. This just
about epitomizes the effort which the average New Zealander puts into
learning about the real
world. Fact. The things which bite you on the bum
in India, are NOT likely to be the things for which you have had shots.
FACT: What might hit you harder on the bum if you go to India now are
two things: India-derived superbugs only discovered in December 2009 -
and the consequences of giving antibiotics like Doxycycline to the
athletes to prevent Malaria, or other antibiotics, to treat infections
while at the Commonwealth Games. Therein lie the real dangers. Let's
look at why:
I've
had all my shots." So said Javelin Thrower Stewart Farquhar. This just
about epitomizes the effort which the average New Zealander puts into
learning about the real
world. Fact. The things which bite you on the bum
in India, are NOT likely to be the things for which you have had shots.
FACT: What might hit you harder on the bum if you go to India now are
two things: India-derived superbugs only discovered in December 2009 -
and the consequences of giving antibiotics like Doxycycline to the
athletes to prevent Malaria, or other antibiotics, to treat infections
while at the Commonwealth Games. Therein lie the real dangers. Let's
look at why:First, Superbugs originating from Inside India. Why has India spawned superbugs? Because ironically, India has a huge culture of over the counter, cheap antibiotics, which are used extensively, and in a way which India specialises in --- which would best be described as --- "haphazard". So while everyone is running around rightly concerned about Dengue "break-neck" fever, what they should be seriously considering is what they might bring back to New Zealand with them. So what the problem with these new bacteria? This:
Even the powerful carbapenems, often reserved for other multi-resistant bugs like methicillin-resistant Staphylococcus aureus (MRSA) and Clostridium difficile, are generally ineffective against bacteria with NDM-1. And experts say there are no new drugs on the horizon to tackle it.
Put simply, if you get a superbug infection in India, not only are you are in shit street, you put everyone else around you in shit streets as well, as well as your family and community when you come home..
"But", I hear you say. "These are fit athletes!" Oh yeah? Fit athletes who have trained to be at their peak will have immune systems at their lowest at the games, for two reasons. Their bodies are stretched to the limit AND they are in a strange country which has a completely different type of "commensal flora" in the community.
And the one thing these athletes depend on is good gut flora, because gut flora is responsible for 70% of your immune system. You know what? Daily Doxycycline to prevent malaria, trashes their commensal flora, something we as a family have had personal experience with.
"Commensal Flora? What's that?" I'm glad you asked, because this is something everyone should know.
Each individual has commensal flora determined by their own environment, what they eat, and the communities in which they live.
Every country has a different circulating "commensal flora" comprising of bacteria, viruses and fungi which emanate from humans, collectively. Even in Western society, that flora is different between countries. So for New Zealanders, say, who travel to Great Britain, there are differences in commensal flora between the countries, which can result, for instance, in the development of boils within a week, in a person whose nutrition and vitamin B levels are borderline.
But India is in a whole different league. Indian commensal flora is radically different to western countries for very obvious reasons. Even Indian doctors I've worked with, tell me that when they go and study overseas for a few years and then return to India to live, the first 18 months will be serial infections until their skin and gut flora re-adjusts back to the "local lifestock". In India, Westerners are behind the eight ball without even trying, because unlike the average Indian, they've never had a chance to adjust to living in or on the periphery of a sewage pit.
And herein lies the second danger which New Zealander athletes and journalists in India. Not only will the daily Doxycycline napalm their gut flora, and compromise their own immune systems which are already stressed,.. AND make them more susceptible to those new superbacteria in India , BUT when they leave, they will effectively spread the superbugs to the four corners of the earth when they leave.
Few people seem to realise what happens to their own internal bacteria, when they use antibiotics. In 2007, in an article called The Sting in the Needle, Dr Peter Collignon, an infectious disease expert, said right at the bottom:
"If you take an antibiotic, it's like napalming your throat"
He only got part of that right. Actually, when you take antibiotics you napalm the whole of your body, the consequences of which can be long term.
The problem with science is that true to the mantra that you only look at something when it smacks you in the face... they have only recently woken up to this problem.
There is one team of awake scientists who have been on to this issue, energetically for some time. In a recently published article, they described people who were given two antibiotic courses, six months apart. The antibiotic used was one which the medical profession said did not affect gut flora. Yet these people suffered significant gut flora trashing, and in some cases, the change in gut flora was permanent. These same authors, four years ago, described antibiotic commensal flora damage as "pervasive". That's not a word you use for a fun joy ride.
Skin infections in India are pretty common, but what happens even in England, when antibiotics are prescribed for skin infections? Big trouble, as shown in this article:
An analysis of UK primary care data found GP prescribing of anti-staphylococcal drugs for skin conditions has soared by 64% in ten years.
Over the same period GP consultations for skin infections rose by 19% and hospital admissions for Staphylococcal aureus increased by 49% - a relationship the UK authors said was unlikely to have arisen ‘by chance’.
Doctors have got to stop being antibiotic prescription automatons.
And parents have to realise that antibiotics should NEVER be used, except in life threatening situations.
Why is this so important for athletes? because, as a recent article showed:..
"Good" Bacteria Keep Immune System Primed To Fight Future Infections, According To Penn Study
28 Jan 2010
Scientists have long pondered the seeming contradiction that taking
broad-spectrum antibiotics over a long period of time can lead to severe
secondary bacterial infections. Now researchers from the University of
Pennsylvania School of Medicine may have figured out why.
The investigators show that "good" bacteria in the gut keep the immune
system primed to more effectively fight infection from invading
pathogenic bacteria. Altering the intricate dynamic between resident and
foreign bacteria - via antibiotics, for example - compromises an
animal's immune response, specifically, the function of white blood
cells called neutrophils.
Senior author Jeffrey Weiser, MD, professor of Microbiology and
Pediatrics, likens these findings to starting a car: It's much easier to
start moving if a car is idling than if its engine is cold. Similarly,
if the immune system is already warmed up, it can better cope with
pathogenic invaders. The implication of these initial findings in
animals, he says, is that prolonged antibiotic use in humans may
effectively throttle down the immune system, such that it is no longer
at peak efficiency.
"Neutrophils are being primed by innate bacterial signals, so they are
ready to go if a microbe invades the body," Weiser explains. "They are
sort of 'idling', and the baseline system is already turned on."
Weiser and first author Thomas Clarke, PhD, a postdoctoral fellow in the
Weiser lab, published their findings last week in Nature Medicine.
"One of the complications of antibiotic therapy is secondary infection,"
Weiser explains. "This is a huge problem in hospitals, but there hasn't
been a mechanistic understanding of how that occurs. We suggest that if
the immune system is on idle, and you treat someone with broad-spectrum
antibiotics, then you turn the system off. The system is deprimed and
will be less efficient at responding quickly to new infections."
The findings also provide a potential explanation for the anecdotal
benefits of probiotic therapies because keeping your immune system
primed by eating foods enhanced with "good" bacteria may help counteract
the negative effects of sickness and antibiotics.
Researchers have for many years understood that most bacteria in the
body are not "bad." In fact, humans (and mice) have a symbiotic
relationship with their resident microbes that significantly impacts,
among other things, metabolism and weight homeostasis. As shown in this
study, microbes also affect the innate immune response, via the cellular
protein Nod1.
Present within neutrophils, Nod1 is a receptor that recognizes parts of
the cell wall of bacteria. Weiser and his colleagues found that
neutrophils derived from mice engineered to lack Nod1 are less effective
at killing two common pathogens, Streptococcus pneumoniae and
Staphylococcus aureus, than neutrophils from mice that do express the
receptor.
In addition, neutrophils from mice that were raised in a germ-free
environment or on antibiotics were likewise diminished in their immune
responses, but this effect was not permanent: Re-exposure of these mice
to a conventional environment (that is, one containing normal bacteria)
restored immune function.
The team provided evidence for a potential mechanism for these
observations by showing that bacterial cell wall material could be
detected in the blood of normal mice, and that it influences neutrophils
in the bone marrow. Finally, the team demonstrated they could improve
immune function by treating both antibiotic-treated mice and human
neutrophils with the Nod1 ligand - a finding that suggests it may be
possible to counter the adverse consequences of antibiotics in humans.
~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~
Antibiotic use, puts the whole community at risk, as this article in May this year said:
Patients whose doctors over-prescribe antibiotics may develop drug resistance that lasts up to a year, putting them and the population at risk when more serious treatment is needed, scientists said on Wednesday.
The more antibiotics are prescribed for coughs and flu-like illnesses, or urine infections, the more bacteria become resistant in a vicious cycle, said British researchers who analyzed 24 previous studies of antibiotic resistance.
"The effect is greatest in the month immediately after treatment, but may last for up to a year, and this residual effect may be a driver for high levels of resistance in the community," said Alastair Hay, a consultant senior lecturer in primary health care at Bristol University, who led the research
Three years ago, strident warnings were being issued;
Antibiotic resistant bugs found in the mouth 6 months after antibiotic use: study.
Last Updated: Friday, February 9, 2007 | 10:03 AM ET
The Canadian Press
Taking a single course of a certain type of antibiotic gives rise to high levels of antibiotic resistant bacteria in the mouth, an effect that lasts for at least half a year, a new study has found.
The extraordinary persistence of the effect startled the scientists who discovered it and others in the field as well, and underscores the need for judicious use of these precious drugs, experts said.
'We were pretty staggered by these data'— Senior author Dr. Herman Goossens
Senior author Dr. Herman Goossens said he and his co-authors assumed that if they followed the subjects in their study for six months they would see the rates of resistant bacteria in their mouths return to normal levels. But that didn't happen.
"We were pretty staggered by these data," said Goossens, a microbiologist at the University of Antwerp, in Belgium. "We never expected this."
Goossens said the findings suggest that even after a single — and short — course of antibiotics, a person could spread resistant strains of bacteria to close contacts within a household or a hospital for months.
The findings, reported Thursday in the journal The Lancet, are a sharp reminder of the power of antibiotics, suggested Eric Brown, a biochemist at McMaster University in Hamilton.
So a quick course of antibiotics and a half a year later, you're still carrying resistant organisms. That's a little bit terrifying," said Brown, whose laboratory is working on alternative ways to kill bacteria, because of the rising problem of antibiotic resistance.
..... "It … should serve as a wake-up call for individual prescribing physicians, nurse practitioners, midwives, dentists and others that inappropriate use of antibiotics does have consequences," said Dr. John Conly, former chair of the Canadian Committee on Antibiotic Resistance and head of the department of medicine at Foothills Medical Centre in Calgary.
~~~~~~~~~~~~~~~~~~~~~
So congratulations, Greg Henderson. I happen to think you've made the right choice for your family. The last thing you need is to bring back superbugs to your wife, family and community.